
by Russell Noga | Updated February 2nd, 2024
Are you questioning the cardiac ablation cost Medicare will cover? Cardiac ablation, a crucial treatment for those with heart rhythm conditions such as atrial fibrillation, comes with significant costs that Medicare often covers, subject to certain conditions. This article cuts through the complexities to provide you with a straightforward explanation of how much Medicare might pay and what out-of-pocket expenses you should be prepared for. Navigate the intricate landscape of healthcare with our guidance on managing costs and maximizing your Medicare benefits for a cardiac ablation procedure.
Key Takeaways
- Medicare covers cardiac ablation when deemed medically necessary, but there are out-of-pocket costs even after insurance, such as 20% of the expenses after deductibles have been met and other additional fees.
- The costs for cardiac ablation procedures can vary widely, with Medicare covering different aspects through Part A (hospital stays), Part B (outpatient services), and Part D (prescription medications), but subscribers still face deductibles, copays, and limitations on coverage.
- Additional insurance options like Medigap and Medicare Advantage plans can help manage costs associated with cardiac ablation, offering benefits like coverage for deductibles, copayments, and coinsurance; however, these come with their own premiums and plan-specific expenses.
Compare 2024 Plans & Rates
Enter Zip Code
Understanding Cardiac Ablation and Medicare Coverage

Atrial fibrillation afib is a medical condition characterized by rapid and irregular beating of the heart’s upper chambers. This might seem benign on the surface, but it carries a significant risk – the potential formation of blood clots that could lead to a stroke. To manage this condition, physicians may employ various treatments, one of which is cardiac ablation – a procedure used to address irregular heart rhythms by eliminating or obstructing problematic heart tissue.
Healthcare providers commonly prescribe medications to control heart rate and anticoagulants like warfarin and direct-acting oral anticoagulants during and after cardiac ablation procedures for AFib. These medications reduce the risk of blood clot formation during treatment, and Medicare covers them when prescribed by a healthcare provider.
Insurance coverage for cardiac ablation isn’t a straightforward ‘yes’ or ‘no’ but involves different aspects, each influenced by various factors. Although it might seem overwhelming, grasping these nuances can significantly help in managing costs.
What is Cardiac Ablation?
Cardiac ablation is a medical procedure employed for the treatment of irregular heartbeats, such as atrial fibrillation, through the removal or obstruction of problematic heart tissue. Atrial fibrillation is a cardiac arrhythmia that can result in more serious complications such as heart failure or stroke. It encompasses various types, including Paroxysmal Afib, Persistent AFib, and Permanent Atrial Fibrillation, each of which may manifest symptoms such as sustained heart palpitations, chest pounding, and irregular heart rhythms.
Cardiac ablation is not a uniform procedure. Various types of ablation procedures are available for atrial fibrillation treatment. These include radiofrequency ablation, which employs heat to eliminate problematic tissue, and catheter ablation, wherein the tissue responsible for arrhythmia is excised during open heart surgery. Understanding these details about cardiac ablation can be instrumental in making informed decisions about your treatment path.
Does Medicare Cover Cardiac Ablation?
Medicare does cover cardiac ablation when it is utilized to obstruct electrical signals that cause an irregular heartbeat and is considered medically necessary for atrial fibrillation treatment. This includes coverage for the procedure itself, as well as related services and medications. Medicare Part D, for instance, provides coverage for medications prescribed by a healthcare provider to treat atrial fibrillation. However, this coverage does not extend to medication taken at home unless you have a prescription drug plan.
While this coverage can be a financial lifesaver, it is important to understand that Medicare generally covers 80% of the expenses related to atrial fibrillation treatments, such as cardiac ablation, once deductibles have been fulfilled. This means that patients may still bear substantial out-of-pocket expenses, which could surpass $15,000.
Obtaining precertification or approval from Medicare before the cardiac ablation procedure can ensure a seamless process and prevent claim rejections. An inaccurate submission of necessary paperwork might lead to claim rejection, which can be appealed. Knowing the coverage details and approval process can help prevent unexpected financial surprises and let you concentrate on recovery.
Breaking Down the Costs: Medicare and Cardiac Ablation

The costs of cardiac ablation can vary depending on your treatment path and the type of Medicare coverage you have. Medicare provides coverage through different parts – Part A, Part B, and Part D, each covering a different facet of your treatment. Understanding these elements can provide a clear picture of what you might expect to pay out of pocket.
If deemed medically necessary, Medicare Part A covers inpatient cardiac ablation. Once you’ve paid the Part A deductible, which is $1,600 in 2023, the treatment costs will be covered. However, patients may still be responsible for copays and other associated fees. Medicare Part D, on the other hand, can provide coverage for medications that are prescribed after cardiac ablation, given that they are considered medically necessary.
The typical cost for cardiac ablation varies from $16,000 to $22,000 for the procedure, accompanied by additional annual maintenance fees that may amount to several thousand dollars per year. It’s important to remember that these costs can vary widely depending on your specific situation and the amount of coverage provided by your Medicare plan.
Medicare Part A and Hospital Stays

When it comes to cardiac ablation, a significant portion of the cost is typically associated with hospital stays. The procedure itself, the necessary follow-up care, and any complications that arise can all result in extended hospital stays. Medicare Part A provides coverage for medically necessary inpatient treatments, such as cardiac ablation, to ensure that beneficiaries receive coverage for the procedure and any required follow-up care during their hospital stay.
While Medicare Part A covers most inpatient hospital costs, you should be aware that you’ll still be accountable for some costs. After the payment of the Part A deductible, you may still need to pay copays and other associated fees. Understanding these costs can help you plan for your treatment and avoid any unexpected expenses.
Moreover, the coverage provided by Medicare Part A is not unlimited. There are limits on the number of days covered in a benefit period, and if you exceed these limits, you may be responsible for a larger portion of your costs. Being aware of these limits can help you better anticipate your potential out-of-pocket costs.
Medicare Part B and Outpatient Services

Outpatient services related to cardiac ablation, such as doctor visits, diagnostic tests, and cardiac rehabilitation programs, are covered by Medicare Part B. This means that you can expect coverage for these services, which are essential to your treatment and recovery.
However, while Medicare Part B provides valuable coverage, it is not without costs. Enrollees are required to pay an annual deductible, which amounted to $233 in 2022, and typically, they are also responsible for covering 20% of the Medicare-approved amount for the outpatient services under Medicare Part B.
It’s also worth noting that Medicare Part B covers diagnostic tests such as electrocardiograms (EKGs) that are used for the assessment of heart health in the setting of cardiac ablation. However, the expenses incurred for these tests may differ based on the location where they are conducted. Understanding these costs can help you plan accordingly and prevent any financial surprises during your treatment. Additionally, it’s important to know whether Medicare cover heart monitors, as these devices can also play a crucial role in monitoring your heart health.
The Role of Medicare Part D

Prescription medications related to cardiac ablation are substantially covered by Medicare Part D. This includes medications that are prescribed after the procedure to manage symptoms and prevent complications, including blood thinners and other necessary drugs.
Medicare Part D has the capability to reduce the cost of medications for AFib treatment, including blood thinners and other drugs prescribed after cardiac ablation, by offering coverage through medical insurance plans. However, the expenses tied to Medicare Part D coverage for these medications can differ based on the specific plan, and individuals generally encounter a copayment ranging from $40 to $170 per month for their drugs.
Enrollment in Medicare Part D can be done through:
- The Medicare Plan Finder
- The plan’s website
- A paper enrollment form
- Contacting the plan directly
- Using the 1-800-MEDICARE number
This will allow you to obtain coverage for medications required for cardiac ablation treatments.
Understanding the role of Medicare Part D in your coverage can help you manage your medication costs and ensure that you have the necessary treatments to support your recovery.
Compare Medicare Plans & Rates in Your Area
Additional Insurance Options to Manage Costs
In addition to the coverage provided by Medicare, there are additional insurance options that can help manage out-of-pocket costs related to cardiac ablation. These options, such as Medigap and Medicare Advantage plans, offer additional coverage that complements Original Medicare. They can cover costs like deductibles, copayments, and coinsurance, helping to reduce your out-of-pocket expenses.
Medigap serves as a supplementary insurance policy designed to alleviate expenses such as deductibles, copayments, and coinsurance for services covered by Original Medicare, including cardiac ablation when deemed medically necessary.
Medicare Advantage plans offer a comprehensive range of benefits, consolidating both Part A and Part B of Original Medicare. These plans frequently include:
- Prescription drug coverage
- Vision services
- Hearing services
- Dental services
However, it’s important to note that these additional insurance options come with their own costs. Premiums, deductibles, and copayments can vary widely depending on the specific plan. Understanding these costs can help you choose the plan that best fits your needs and budget.
Medigap: Supplementing Your Medicare Coverage
Medigap, a form of supplementary insurance, aids individuals in covering certain out-of-pocket expenses not included in Medicare coverage, such as copays, deductibles, and coinsurance. Additionally, it may extend coverage to medical treatment obtained while traveling outside of the United States.
Indeed, Medicare Supplement Plans provided by private insurance companies have the capability to help medicare cover atrial fibrillation by assisting with coinsurances, deductibles, or copayments for treatments. It is important to note that enrollment in these plans is guaranteed only during specific periods or under certain conditions.
A pre-existing condition refers to a health issue that an individual has before enrolling in a health plan. In the context of Medigap and AFib, it may result in a higher monthly premium or even denial of coverage. However, having prior insurance coverage generally means that pre-existing limitations will not apply.
Understanding these details can help you make informed decisions about whether Medigap is the right choice for you.
Medicare Advantage Plans: An Alternative Path
Offering an alternative to Original Medicare, Medicare Advantage plans, also referred to as Medicare Part C, are available. These plans are offered by a private insurance company approved by Medicare and often include prescription drug coverage and additional benefits beyond those offered by Original Medicare.
Medicare Advantage plans that incorporate prescription drug coverage will assist in covering the expenses for prescription drugs, including AFib medications. This can be a significant benefit for individuals who require regular prescriptions for their condition.
However, like Medigap, Medicare Advantage plans come with their own costs. A Medicare Advantage plan with prescription drug coverage typically costs around $36 per month in premiums. This coverage option can provide comprehensive care and help lower medication expenses for members. Understanding these costs can help you decide whether a Medicare Advantage plan is the right choice for you.
Financial Assistance and Support Programs
While Medicare and additional insurance options can provide significant coverage for cardiac ablation, there may still be substantial out-of-pocket costs. For those who need additional assistance, there are financial assistance programs available, including:
- The Patient Access Network (PAN) Foundation, which provides support for individuals with heart failure
- Another fund that offers a one-time $500 grant for those with heart valve disorders
- The HealthWell Foundation, which provides copayment or premium assistance for Medicare beneficiaries with cardiomyopathy
These programs can help alleviate the financial burden of cardiac ablation.
Extra Help is a program designed to provide financial assistance for prescription medication expenses to individuals with low income. This can be particularly advantageous for those who require frequent prescriptions after medical procedures such as cardiac ablation. In 2024, individuals with a monthly income up to $1,843 ($2,485 for couples) and assets below specified limits may qualify for this financial aid.
These financial assistance programs can provide significant relief for individuals facing high cardiac ablation costs. However, it’s important to understand the eligibility criteria and application process for each program. With this knowledge, you can find the assistance that best meets your needs and navigate the path to recovery with less financial stress.
Planning Ahead: What to Ask Your Healthcare Provider
Advance planning is vital for managing the costs associated with cardiac ablation. This includes having conversations about insurance coverage and costs with your healthcare provider before the procedure. Engaging in a discussion about insurance coverage before undergoing a cardiac ablation procedure holds great significance in gaining clarity on your financial obligations and reducing unexpected expenses associated with medical bills.
There are several essential questions to consider asking your healthcare provider. These include inquiries about:
- The cost of cardiac ablation
- Factors that can impact the cost
- Insurance coverage
- Additional expenses
- Available financial aid programs
- Possibilities to negotiate or lower the cost
- Alternative cost-efficient treatments
- A breakdown of the costs
- Any follow-up or ongoing expenses post the procedure.
Asking these questions can provide you with a clear picture of the estimated cost range for your procedure, which can range from $21,000 to $50,000, and help you plan accordingly. Understanding these costs can help you plan for your treatment and ensure that you have the necessary resources to support your recovery.
Navigating the Approval Process for Cardiac Ablation
The approval process for cardiac ablation can be intricate, but comprehending the process can facilitate a smooth experience. In order to receive coverage for cardiac ablation under Medicare, a referral from a doctor is required. The doctor’s involvement is essential in submitting the required documentation for approval based on the patient’s medical needs.
Medicare will provide coverage for cardiac ablation if a physician determines that the treatment is medically necessary. This assessment plays a critical role in determining whether Medicare will authorize and reimburse for the procedure.
The duration of Medicare’s approval process for cardiac ablation can vary significantly; however, on average, it may take approximately 741 days from the AF diagnosis to the ablation referral. Understanding this process can help you plan your treatment timeline and ensure that you have the necessary approval in place before your procedure.
Summary
In conclusion, understanding the costs and coverage of cardiac ablation under Medicare can be complex, but it’s an essential part of planning for your treatment. With knowledge of the different parts of Medicare, additional insurance options, and financial assistance programs, you can navigate your path to recovery with confidence. Remember, the journey may seem daunting, but with the right knowledge and preparation, you can focus on what truly matters – your recovery and ongoing heart health.
Compare 2024 Plans & Rates
Enter Zip Code
Frequently Asked Questions
What is the average cost of a cardiac ablation?
The average cost of a cardiac ablation can range from $10,000 to $50,000, influenced by factors such as complexity of the case, hospital charges, and geographic location.
Will insurance pay for an ablation?
Yes, insurance may cover ablation, but it depends on specific conditions and the type of pain being treated. It’s more likely to be covered for facet joint pain if all conditions are satisfied.
Is ablation for AFib worth it?
Ablation for atrial fibrillation may be a good option for those with AFib lasting 7 days or less and no other structural heart problems, but it may be less effective for those with more persistent AFib. Research shows it stops AFib in 60 to 80 out of 100 cases for 6 to 12 months.
What is cardiac ablation and why is it necessary?
Cardiac ablation is a necessary medical procedure for treating irregular heartbeats like atrial fibrillation by removing or blocking problematic heart tissue, especially when other treatments have been ineffective.
Are there financial assistance programs available for individuals facing high cardiac ablation costs?
Yes, there are financial assistance programs available, such as the Patient Access Network (PAN) Foundation and Extra Help, to provide support for eligible individuals facing high cardiac ablation costs.
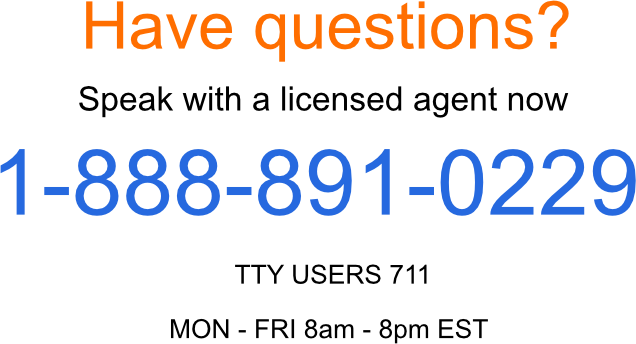
Speak to the Professionals about Medigap Plans and Original Medicare
If you find understanding the benefits involved with Original Medicare and Medigap Plans challenging, you’re not alone. Whether it’s a Medigap plan, or you want to know more about Medicare coverage for cardiac ablation, we can help. Call our team at 1-888-891-0229 for a free consultation or complete the contact form on this site, and an expert will call you back at a convenient time.
We have decades of experience advising our clients on the complexities of Medicare and Medigap plans, the benefits, cost and deductibles. We’ll ensure you get the best rate in your state and advice you can trust.
Russell Noga is the CEO and Medicare editor of Medisupps.com. His 15 years of experience in the Medicare insurance market includes being a licensed Medicare insurance broker in all 50 states. He is frequently featured as a featured as a keynote Medicare event speaker, has authored hundreds of Medicare content pages, and hosts the very popular Medisupps.com Medicare Youtube channel. His expertise includes Medicare, Medigap insurance, Medicare Advantage plans, and Medicare Part D.

