
by Russell Noga | Updated March 23rd, 2024
As we head into 2025, understanding the shifts in Medigap plans could save you from unforeseen costs and coverage hiccups. This article hones in on the essential information about Medigap plans 2025, spotlighting plans like G and N, and unpacks the latest on eligibility rules and state-specific legislation—all to help you make an informed choice without hassle or confusion.
Key Takeaways
- Significant changes to Medigap access and premium restrictions are expected in 2025, especially for beneficiaries under 65 in states considering new legislation.
- Medicare Plans G and N, the high-deductible Plan G, and Plan F (for those who were eligible before January 1, 2020) will be the most sought-after Medigap plans in 2025, offering comprehensive coverage and a safety net against unexpected medical costs.
- State-specific regulations greatly influence Medigap plan availability, premiums, and consumer protections, making it crucial for beneficiaries to understand their state’s specific Medigap regulations and options for financial assistance.
Compare 2025 Plans & Rates
Enter Zip Code
Navigating Medigap Changes in 2025
The Medicare landscape is predicted to undergo significant shifts in 2025, redefining the Medigap space. With legislation underway in states like Ohio, Nebraska, and Iowa, access to Medigap plans for beneficiaries under 65 is set to improve.
This move towards inclusivity aims to align premium restrictions with costs for those 65 and over, ensuring a fairer Medicare ecosystem for all.
The Best Medicare Supplement Plans for 2025

Four Medigap plans are anticipated to stand out in the new year due to their comprehensive coverage and value. Medicare Plans G and N, the high-deductible Plan G, and Plan F (for those who qualify) are set to be the most popular Medigap plans in 2025. From covering copayments and deductibles to offering additional benefits, these plans provide a safety net against unexpected medical costs.
Medicare Plan G in 2025 – The most popular
Beneficiaries favor Medicare Plan G for its comprehensive coverage. Available to individuals new to Medicare from January 1, 2020, it offers a high-deductible version with an annual deductible set at $2,800 for 2024, hinting at a similar trend for 2025.
The Centers for Medicare & Medicaid Services (CMS) has proposed updates to Medicare Advantage payment growth rates and changes to the Medicare Advantage and Part D payment methodologies, which may also impact Plan G premiums and coverage.
Medicare Plan N for 2025 – Great savings and coverage

In 2025, Medicare Plan N will be highlighted for its potential savings and comprehensive coverage. With CMS proposing updates for Medicare Advantage and Part D programs, the premiums and costs of Medigap plans like Plan N are set to be affected. These updates include the continued phase-in of the updated Medicare Advantage risk adjustment model and changes to the Medicare Advantage Plan Risk Adjustment Data Validation (RADV) appeals process, which could impact the financial performance of Medicare Advantage plans and, subsequently, the market dynamics for Medigap plans like Plan N.
High-deductible Plan G
Another popular choice, High-deductible Plan G, provides lower premiums but demands a higher annual out-of-pocket limit. This plan is particularly attractive to individuals who prefer to pay lower premiums and are comfortable with the possibility of higher out-of-pocket expenses. However, the annual deductible amount for high-deductible Plan G is adjusted yearly based on the Consumer Price Index for all Urban Consumers (CPI-U), making it essential to stay updated on these changes.
Medicare Plan F – Do you qualify?
Renowned for its comprehensive coverage, Medicare Plan F is exclusively available to beneficiaries who qualified for Medicare before January 1, 2020. For these individuals, Plan F remains a viable option, offering coverage for a wide range of Medicare cost-sharing, including:
- the annual Part B deductible
- Part B coinsurance and copayments
- Part A coinsurance and hospital costs
- skilled nursing facility coinsurance
- Part A hospice care coinsurance or copayment
- Part A deductible
- foreign travel emergency coverage
However, due to the MACRA Act, beneficiaries who became eligible for Medicare on or after January 1, 2020, are not eligible for Medigap Plan F.
Understanding New Eligibility Criteria
States vary in their eligibility criteria for Medigap plans. Some states, including Ohio and Nebraska, are considering legislation to improve Medigap access for beneficiaries under 65. Such legislative changes could require Medigap insurers to offer all their plans to newly eligible beneficiaries regardless of age while imposing restrictions on premiums charged.
Exploring Coverage Enhancements
Known for its extensive coverage, Medigap Plan F includes coinsurance, hospital costs post-Medicare benefits, and Part B coinsurance or copayment. Plan F also offers additional perks, such as foreign travel emergency health care coverage, making it a popular choice among beneficiaries with chronic health conditions. However, Plan F does not cover prescription medications from a pharmacy, necessitating a separate Part D plan for this coverage.
Adjustments to Premiums and Costs
The individual’s location and the insurer’s pricing methods can cause variations in Medigap, including Plan F, premiums. The annual deductible amount for high deductible versions of Medigap Plans F and G will be $2,800 effective January 1, 2024, with CMS adjusting this deductible amount based on the Consumer Price Index for all Urban Consumers (CPI-U). Therefore, careful attention to these factors is crucial when considering Plan F.
State-Specific Medigap Variations
State-specific regulations significantly impact the Medigap landscape. With no federal guarantees for Medigap enrollment for those under 65, states have the authority to pass legislation that would provide the guaranteed issue of these policies. However, beneficiaries in states lacking Medigap consumer protections can be denied coverage or charged higher premiums due to preexisting conditions.
This disparity underscores the importance of understanding your state’s specific Medigap regulations.
States Expanding Medigap Access
Several states are advancing efforts to enhance Medigap access. For instance, Arkansas, California, and Connecticut now require Medigap insurers to offer all their plans to newly eligible beneficiaries regardless of age. Additionally, states like Ohio and Nebraska are considering legislation to improve Medigap access for beneficiaries under 65.
These initiatives highlight the growing efforts to make Medigap more inclusive and accessible.
Premium Considerations by State
State variations significantly influence premium considerations for Medigap plans. Premium variations can significantly depend on whether a state uses community rating, issue-age rating, or attained-age rating systems. Also, some states allow for premium adjustments based on factors such as smoking status, gender, and residential area, adding another layer of variability to Medigap premiums.
Therefore, it’s important for beneficiaries to understand these state-specific premium considerations when choosing a Medigap plan.
Barriers to Medigap Enrollment
Despite advancements in Medigap access, enrollment barriers persist for beneficiaries. These include a lack of federal guarantees, state-specific regulations, and challenges in accessing affordable coverage.
For instance, attempts to expand Medigap access for beneficiaries under 65 through state legislation have failed in states like Arizona and Texas. Also, beneficiaries in states lacking Medigap consumer protections can be denied coverage or charged higher premiums due to preexisting conditions.
Compare Medicare Plans & Rates in Your Area
Comparing Medigap Plans for Optimal Coverage
A meticulous comparison of available options is necessary to choose the right Medigap plan. It’s important to evaluate the benefits and features of each plan, their cost-sharing requirements, and potential future changes in coverage. While all Medigap plans are required by law to provide certain basic benefits, certain Medigap plans may offer additional perks, such as foreign travel emergency health care coverage.
Plan Benefits and Features Comparison
Understanding the distinct features of each plan is crucial when comparing Medigap plans. For instance, Medigap Plan A provides core benefits but does not cover the Part A and B deductibles or foreign travel emergency costs. On the other hand, Medigap Plan G provides extensive coverage, including coinsurance costs for Part A and B, blood (first 3 pints), Part A hospice care, skilled nursing facility care, and 80% foreign travel exchange after deductibles. Understanding these distinct features will help beneficiaries select a plan that best suits their needs.
Evaluating Cost-Sharing Requirements
Grasping cost-sharing requirements is integral to the Medigap plan selection process. All Medigap plans standardize their cost-sharing for covered services, although some plans offer lower out-of-pocket costs in exchange for higher premiums. Therefore, it’s important to compare these cost-sharing requirements to choose a plan that offers the most value.
Tips for Choosing the Right Plan
Selecting the right Medigap plan necessitates:
- A thoughtful analysis of personal needs
- Potential future healthcare expenses
- A detailed comparison of monthly premiums against other out-of-pocket costs like deductibles and copayments
- Ensuring that the insurance company offering the Medigap plan has a strong financial stability score, indicating its reliability and longevity in the market.
Financial Assistance and Subsidies for Medigap Enrollees
Financial assistance programs are pivotal in managing Medigap expenses. Beneficiaries may be eligible for subsidies that can lower their prescription drug costs or assist with other Medigap-related costs. These programs, such as the Low-Income Subsidy (LIS) Program, state assistance programs, and non-profit organizations, can provide much-needed relief for beneficiaries struggling with healthcare costs.
Low-Income Subsidy (LIS) Program Expansion
The Part D Low-Income Subsidy (LIS) Program, also referred to as Extra Help, is slated for expanded coverage starting in 2024 to benefit more beneficiaries. With the expansion, individuals earning up to 150% of the federal poverty level and having resources within specified limits will be eligible for full LIS benefits.
The Medicare Advantage Program assists eligible Medicare beneficiaries by covering costs such as premiums, deductibles, and coinsurance for their prescription drug plans.
Additional Programs for Cost Relief
Other financial assistance programs, alongside the LIS program, can offer further cost relief for Medigap enrollees. State Pharmaceutical Assistance Programs (SPAPs) help eligible residents pay for prescription drugs, and they coordinate with Medicare Part D. Pharmaceutical companies offer Pharmaceutical Assistance Programs (PAPs), which provide medications at a reduced cost or for free to individuals meeting certain income or insurance criteria.
Non-profit organizations and charitable foundations may offer financial assistance or grants to cover the cost of Medigap premiums and out-of-pocket expenses for qualifying individuals.
Navigating Assistance Eligibility
Grasping the eligibility requirements for assistance programs can aid beneficiaries in maximizing their access to these resources. For example, eligibility for Medigap assistance programs generally requires enrollment in both Medicare Part A and Part B, with the inability of Medicare Part C enrollees to purchase Medigap policies.
Also, individuals under the age of 65 who are on Medicare due to disability or end-stage renal disease may face restrictions when trying to purchase a Medigap policy before they turn 65, depending on the state they live in.
The Interplay Between Medigap and Medicare Advantage Plans 2025
Serving different purposes, Medigap and Medicare Advantage plans cater to varied healthcare needs. While Medigap plans to provide Medicare supplement insurance that covers costs not paid by Original Medicare, Medicare Advantage is an alternative to receiving Medicare benefits. It often includes additional services like vision or dental care.
It’s important to note that beneficiaries are not allowed to have both a Medigap policy and a Medicare Advantage plan simultaneously.
Distinct Features of Each Plan Type
Both Medigap and Medicare Advantage plans have their unique features. For instance, unlike Medicare Advantage plans, which may restrict provider access and require referrals to see specialists, Medigap plans allow beneficiaries the freedom to choose healthcare providers without referrals. Also, while Medicare Advantage plans often include prescription drug coverage, enrollees of Medigap plans are required to obtain an additional prescription drug plan to avoid penalties.
Understanding these distinct features will help beneficiaries make an informed decision between the two plan types.
Making the Switch: Considerations and Processes
A thoughtful evaluation is required when switching between Medigap and Medicare Advantage plans. Beneficiaries may face difficulties obtaining Medigap coverage after leaving Medicare Advantage, especially in states without guaranteed-issue rights. For instance, beneficiaries in states lacking Medigap consumer protections can be denied coverage or charged higher premiums due to preexisting conditions.
Therefore, switching between Medigap and Medicare Advantage must be carefully considered.
Impact on Prescription Drug Coverage
Choosing between Medigap and Medicare Advantage can influence prescription drug coverage too, especially with drug costs high. For instance, Medicare Part D will see substantial changes in 2025, such as a new $2,000 out-of-pocket spending cap, the elimination of the coverage gap, and a new option allowing Part D enrollees to spread costs over the year, which could lead to lower prescription drug costs.
Understanding these changes and how they interact with Medigap and Medicare Advantage plans will help beneficiaries ensure they have adequate prescription drug coverage.
Preparing for Medigap Enrollment in 2025
When it comes to Medigap enrollment, preparation is vital. Understanding the enrollment timeline, gathering the necessary documents, and avoiding common pitfalls can make the process smoother. For instance, the Medigap open enrollment period starts on the first day of the month a person turns 65 or older and is enrolled in Medicare Part B, and it lasts for six months. During this period, insurance companies cannot deny coverage or charge more based on health status.
Enrollment Timeline for 2025
The Medigap open enrollment period is an essential window for beneficiaries to ensure their coverage. This 6-month period begins the first month you have Medicare Part B, and you are 65 or older. During this period, insurance companies cannot deny coverage or charge more based on health status.
Thus, understanding this enrollment timeline is essential to avoid missing out on this period of guaranteed coverage.
Documents and Information Needed
For Medigap plan enrollment, beneficiaries are required to provide personal identification, such as a driver’s license or passport, and a copy of their Medicare card to validate their current Medicare coverage. Having these documents on hand can simplify the enrollment process and ensure a smooth transition to Medigap coverage.
Avoiding Common Enrollment Pitfalls
Dodging common pitfalls in the Medigap enrollment process can spare beneficiaries time and frustration. For instance, beneficiaries should remember that they cannot have both a Medigap policy and a Medicare Advantage plan simultaneously. Furthermore, individuals under the age of 65 who are on Medicare due to disability or end-stage renal disease may face restrictions when trying to purchase a Medigap policy before they turn 65, depending on the state they live in.
Summary
Navigating the changes to Medigap policies in 2025 may seem daunting, but with the right knowledge and preparation, it can be a manageable task. From understanding the best Medicare Supplement Plans for 2025 and how states are working to expand Medigap access to comparing plans and preparing for enrollment, this guide has equipped you with the necessary knowledge to make informed decisions. Remember, choosing the right Medigap plan is an investment in your health and peace of mind.
Compare 2025 Plans & Rates
Enter Zip Code
Frequently Asked Questions
What are the best Medicare Supplement Plans for 2025?
The best Medicare Supplement Plans for 2025 are Plan G, Plan N, High-deductible Plan G, and Plan F for those who qualify. Consider these options when making your decision.
How are premiums for Medigap plans determined?
The premiums for Medigap plans are determined by the individual’s location and the pricing methods used by the insurance company. These factors can cause wide variations in premium costs.
Can I have both a Medigap policy and a Medicare Advantage plan simultaneously?
No, you are not allowed to have both a Medigap policy and a Medicare Advantage plan simultaneously.
What is the Medigap open enrollment period?
The Medigap open enrollment period begins on the first day of the month you turn 65 or older and are enrolled in Medicare Part B, lasting for six months. After this period, insurance companies can use medical underwriting to decide whether to accept your application or not.
What documents do I need to enroll in a Medigap plan?
You will need personal identification like a driver’s license, passport, and a copy of your Medicare card to enroll in a Medigap plan. This will verify your current Medicare coverage.
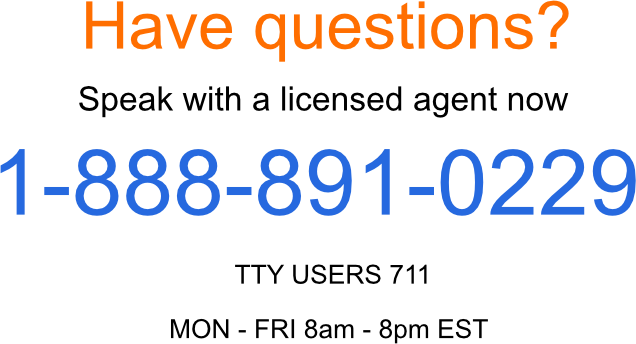
Speak to the Professionals about Medigap Plans and Original Medicare
If you find understanding the benefits involved with Original Medicare and Medigap Plans challenging, you’re not alone. Whether it’s a Medigap plan, or you want to know more about the Best Medigap Plans in 2025, we can help. Call our team at 1-888-891-0229 for a free consultation or complete the contact form on this site, and an expert will call you back at a convenient time.
We have decades of experience advising our clients on the complexities of Medicare and Medigap plans, the benefits, cost and deductibles. We’ll ensure you get the best rate in your state and advice you can trust.
Russell Noga is the CEO and Medicare editor of Medisupps.com. His 15 years of experience in the Medicare insurance market includes being a licensed Medicare insurance broker in all 50 states. He is frequently featured as a featured as a keynote Medicare event speaker, has authored hundreds of Medicare content pages, and hosts the very popular Medisupps.com Medicare Youtube channel. His expertise includes Medicare, Medigap insurance, Medicare Advantage plans, and Medicare Part D.


